The loneliness pandemic among our nation’s elderly — and its connection to the coronavirus pandemic
It’s a sad fact that half of U.S. nursing home residents die within five months before dying — in normal times — which means that a substantial number of nursing home deaths counted as Covid-19 deaths may have been due to other causes rather than the virus. A significant cause of death for the elderly and particularly in nursing homes, even in normal times, is social isolation and consequent loneliness and loss of will to live, which is a bigger killer than obesity and air pollution. These forces have been massively exacerbated by the coronavirus pandemic and resulting social distancing policies.
[I offer these thoughts as speculations in trying to understand the nature of the pandemic better. This essay offers no strong conclusions, just suggestions based on current data. As more data comes in I’ll revise this piece accordingly. Last update: 9/30/20]
Even before the coronavirus pandemic, loneliness was already a more serious killer of the elderly than obesity or air pollution. It’s been made far worse by the pandemic and lockdown policies that have eliminated family visits in a large number of nursing homes around the country.
Our elderly are literally dying, in large numbers, from loneliness, which translates physically into losing the will to live and increased dementia, Alzheimer’s, heart disease, cancer, and other direct causes of death. Loneliness and depression make all of these ailments more serious and strongly affects the ability to survive. The subtitle to a recent New York Times article (Aug. 16, 2020) says it all: “Struck hard by the pandemic, long-term and assisted living facilities shut their doors to outsiders. Many still have not reopened.”
Toby Edelman, a public policy attorney and advocate for better elder care, stated in testimony before Congress in July of 2020 (emphasis added): “Residents’ rights, including the right to participate in in-person resident groups, to eat in the dining room [have been eliminated]. (Many residents are largely confined to their rooms, with the doors closed).”
It is not at all difficult to understand how we’ve seen such a large increase in Alzheimer’s deaths, and other deaths that mostly afflict the elderly, when such a large population is subjected to essentially solitary confinement, the worst punishment that even jailed prisoners are subjected to because it quickly saps the will to live.
We also learned recently that nursing homes were heavily incentivized to evict (“involuntary discharges”) normal patients in order to take in new coronavirus patients. Nursing homes are paid “at least $600 more a day in Medicare dollars than people with relatively mild health issues, according to nursing home executives and state officials.” This is serious new revenue.
We also learned in the same story that the governors of not only New York (which we knew already) but also a dozen other governors, including Pennsylvania, New Jersey, and California, urged and in many cases ordered (via executive order) nursing homes to take in coronavirus patients from hospitals in order to clear up ICU and other types of hospital beds. This policy direction from the governors may have seemed reasonable and responsible in the early days of the pandemic but it quickly became clear that it led to a disaster in terms of infecting large numbers of nursing home residents, who we know now are probably the most vulnerable to the virus — regardless of whether they died directly from the virus or not.
A September article from Politico examined the unfortunate rise in dementia and Alzheimer’s deaths in the U.S., almost all of which have occurred in nursing homes:
“There’s something wrong, there’s something going on and it needs to be sorted out,” Robert Anderson, chief of mortality statistics at the CDC, said in a recent interview. “This is highly unusual.”
It’s the second time this year that deaths from other causes have spiked in tandem with a coronavirus wave. The first occurred early in the pandemic and was attributed to dementia as well as heart disease and pneumonia. The second cycle is attributed almost entirely to dementia — 61,000 deaths since June, which is 11,000 more than usual in that time frame. That large number is raising alarm over the immense difficulty of taking care of these patients in a pandemic, the conditions in long-term care facilities and the government’s lagging efforts to bolster them.
As the U.S. passes 160,000 reported deaths from the pandemic it’s important to understand how and why coronavirus deaths are occurring. Almost one half of all deaths attributed to Covid-19 are from U.S. nursing home populations, mostly patients but some staff also.

A large majority of Covid-19 hospitalizations and deaths have occurred in patients with two or more comorbidities, which are defined as serious illnesses or conditions that existed before the virus was contracted. For example, a study of New York City’s Covid-19 hospitalizations found that 88% had two or more chronic comorbidities and 94% had at least one comorbidity. Most had high blood pressure (major risk factor for heart attacks), diabetes, or obesity. And loneliness — a major cause of death in normal times, is, unsurprisingly very common in nursing homes.
A study of Italy’s (another major Covid-19 hotspot for deaths) dead found similar results. Italy’s health minister stated, based on the study that “only 12 percent of death certificates have shown a direct causality from coronavirus.” Direct causality means that the medical professional assessing the cause of death could say with some confidence it was the virus that caused the death, rather than “dying with” Covid-19.
“Dying with” Covid-19 means that the patient had the virus but likely died from a comorbidity or other cause.
U.S. CDC death reporting guidelines (“Guidance for Certifying Deaths Due to Coronavirus Disease 2019 (COVID–19") encourage medical professionals to report the cause of death as Covid-19 if there is reason to believe the virus was implicated. No test is required. The Guidelines state:
In cases where a definite diagnosis of COVID–19 cannot be made, but it is suspected or likely (e.g., the circumstances are compelling within a reasonable degree of certainty), it is acceptable to report COVID–19 on a death certificate as “probable” or “presumed.” In these instances, certifiers should use their best clinical judgement in determining if a COVID–19 infection was likely. However, please note that testing for COVID–19 should be conducted whenever possible.
This is why the fineprint for websites that show reported Covid-19 deaths in the US and many other countries says “reported or probable.” “Probable” refers to death reporting under this part of the CDC guidelines.
The reason for this erring on the side of inclusion, as reported by Dr. Deborah Birx, the White House’s Coronavirus Response Coordinator, is to better understand the possible dynamics of the disease.
But this erring on the side of inclusion risks significant over-counting of deaths. And that over-counting can lead to unwarranted policy responses that can cause significant harm themselves, such as exacerbating quite significantly the already very high death rates in nursing homes, from increased loneliness, increased dementia and associated problems, as well as from the virus itself.
Counting nursing home deaths
1.3 million Americans lived in nursing homes in 2015, and in normal times half of those people die within five months from normal causes of death that afflict elderly populations. Five months is the median time before death; the average is longer because some patients last far longer before succumbing. 65% die within one year of admission.
That’s during normal times.
Half of this 1.3 million population would have died in normal times within five months (this is what it means that five months is the median survival time), equaling approximately 0.65 million deaths.
5 months is approximately the time it’s been since the pandemic hit the U.S. in force.
The U.S. is counting in its official statistics not only those people who die “from” Covid-19, but also those who die “with” Covid-19, as discussed above, based on CDC guidelines encouraging known and “probable” Covid-19 deaths.
I showed above that about half of the approximately 160,000 Covid-19 deaths so far (as of mid-August, 2020) are from nursing home populations, totaling about 80,000.
When we compare the approximately 80,000 nursing home deaths attributed to Covid-19 (either “from” or “with” Covid-19, because the data available don’t always distinguish these key details) we see that there would be over 8 times that many deaths (0.65 million divided by 80,000 = 8.125) from all other causes in the nursing home population during normal times.
It is not difficult to see how the U.S. could be significantly over-counting Covid-19 deaths because we have an 8:1 higher normal death rate in normal times as compared to the reported nursing home death rate attributed to Covid-19, including “probable” deaths.
In other words, during the time that we have seen approximately 80,000 nursing home deaths associated with Covid-19 in the last 5 months we would in normal times have seen about 0.65 million deaths from all causes among the same population.
There is a chance that a large number of the nursing home Covid-19 deaths did in fact result “from” the virus, rather than other causes. But it seems likely that many of the deaths, perhaps a large portion, associated with Covid-19 would have happened anyway, from other causes, when we consider the five-month normal median survival time for nursing home patients, plus the data about two or more comorbidities in 90% of covid-19 hospitalizations and/or deaths.
We will need, however, an excess deaths study specific to U.S. nursing home populations to arrive at a more clear understanding. More on this below.
What about excess deaths data?
Heart disease is the most common cause of death during normal times, with fully 1 in 4 of all American deaths coming from heart disease, according to the CDC. This totals about 647,000 Americans dying each year from heart disease alone (four times the current official death toll from the pandemic). This would be about 260,000 deaths from heart disease in a 5 month period in normal times.
Eight medical groups in the U.S. issued a statement in April warning about people avoiding hospitals because of fears of the virus, which may lead to higher deaths from heart attacks, strokes and cardiac arrest during the pandemic and governmental responses to the pandemic.
Excess deaths figures aggregated by CDC show that there is clearly a much higher death rate for 2020 for the overall population (Figure 2), but it is not the case that all of these excess deaths are caused by the virus.

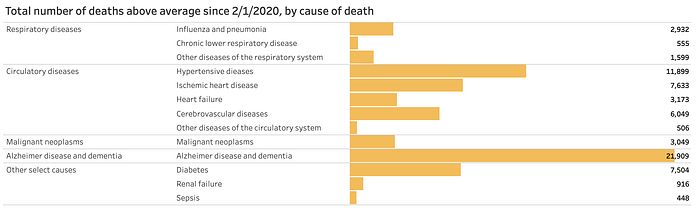
A large number of excess deaths are due to causes other than COVID-19, as CDC’s data also show (Figure 3). These non-COVID-19 excess deaths total over 70,000 deaths — almost half of the total excess deaths reported in the U.S. so far (as of early August, 2020). By far the single largest excess death category is Alzheimer’s and dementia — the area particularly relevant to nursing home populations.
Most of these excess deaths, and perhaps all, were arguably caused by the media and policy responses to the novel coronavirus — not the virus itself — exacerbating underlying conditions, limiting hospital access, increasing loneliness and dementia, particularly in nursing home populations, and other causes.
A key disclaimer for this data is this statement from the CDC web page “methods” section: “Deaths with an underlying cause of death of COVID-19 are not included in these estimates of deaths due to other causes…. For the majority of deaths where COVID-19 is reported on the death certificate (approximately 95%), COVID-19 is selected as the underlying cause of death.”
So this CDC analysis of excess deaths does not take into account the fact that medical professionals were heavily influenced by NVSS guidelines and other factors to list COVID-19 as an underlying cause of death “more often than not” (as the March 24 NVSS report stated). Apparently these guidelines led to “more often than not” being 95% of the time. Accordingly, there is yet another significant data quality issue with CDC’s data on excess deaths from non-COVID-19 causes.
Last, in terms of explaining the excess deaths figures, it could still be the case that there are excess deaths resulting from the virus that aren’t being reported, for various reasons, but also that nursing home Covid-19 deaths are being over-reported. These two conclusions are not mutually exclusive.
There have been no excess deaths studies specific to nursing homes in the U.S., to my knowledge, and this would be helpful data in understanding whether what I’ve suggested here is accurate. My rough analysis of the median survival rate of nursing home patients compared to the reported nursing home deaths is a simple kind of excess deaths analysis.
One study looking at nursing home excess deaths in England and Wales for March and April of 2020, found approximately 20,000 excess deaths for these populations, which if mirrored in the U.S. would cast serious doubt on the hypothesis I’ve pursued in this piece. Such studies still raise questions about the underlying cause of death because it is possible that much of the excess deaths even in nursing home populations may be indirectly related or unrelated to the coronavirus.
In closing, it seems likely, given the underlying death rates plus official reporting guidelines, that we may be seeing a significant inflation of Covid-19 deaths for nursing home populations.
We’ll learn much more as comprehensive health data arrives in the coming months and years, and particularly as Covid-19 death reports are re-analyzed.
